Hospitals are complex healthcare environments that depend on a wide range of equipment to deliver quality care, save lives, and ensure patient safety. Whether it’s a life-saving defibrillator or a basic thermometer, every piece of hospital equipment plays a critical role in diagnosis, treatment, and recovery.
This guide explores the essential equipment found in hospitals, their purposes, classifications, and how they support clinical care. For healthcare professionals, patients, and caregivers, understanding this equipment enhances awareness and fosters trust in the medical system.
What Is Hospital Equipment?
Definition
Hospital equipment refers to the devices, instruments, and tools used in a medical facility to support patient care, diagnosis, monitoring, and treatment. These tools range from simple manual instruments to highly sophisticated computerized machines.
Categories of Equipment
Hospital equipment can be broadly classified into:
- Diagnostic equipment
- Therapeutic equipment
- Monitoring equipment
- Surgical equipment
- Durable medical equipment (DME)
- Support and utility equipment
Each category serves a specific function and contributes to different aspects of healthcare delivery.
Diagnostic Equipment
Diagnostic equipment helps medical professionals identify the cause of a patient’s symptoms and make accurate diagnoses.
1. X-Ray Machines
Used for imaging bones, joints, and internal organs. Commonly used in trauma and orthopedic departments.
2. MRI Scanners
Provides detailed images of soft tissues such as the brain, spinal cord, and muscles without using radiation.
3. CT Scanners (Computed Tomography)
Combines X-ray images to create cross-sectional views, often used for detecting tumors, fractures, and internal bleeding.
4. Ultrasound Machines
Uses sound waves to produce images of internal body structures, frequently used in pregnancy and abdominal scans.
5. ECG (Electrocardiogram) Machines
Records the electrical activity of the heart to detect arrhythmias or cardiac damage.
6. Laboratory Analyzers
Used in pathology labs for testing blood, urine, and other samples for infection, glucose, cholesterol, or other abnormalities.
Monitoring Equipment
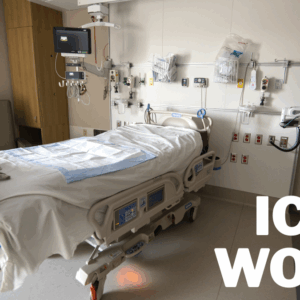
Monitoring equipment continuously tracks a patient’s vital signs and physical condition, especially in ICUs and surgical wards.
1. Vital Signs Monitors
Displays heart rate, blood pressure, oxygen saturation (SpO2), and temperature.
2. Cardiac Monitors
Used in critical care units to track the electrical activity of the heart in real-time.
3. Pulse Oximeters
A non-invasive device clipped on the finger to measure blood oxygen levels and pulse.
4. Capnography Machines
Monitors carbon dioxide levels in exhaled air, essential during anesthesia and critical care.
Therapeutic Equipment
This equipment is used for treating medical conditions or supporting the body’s function during or after illness.
1. Infusion Pumps
Delivers fluids, medication, or nutrients intravenously in controlled amounts.
2. Defibrillators
Sends electrical shocks to the heart during cardiac arrest to restore normal rhythm.
3. Ventilators
Supports or replaces spontaneous breathing for patients with respiratory failure.
4. Dialysis Machines
Filters and purifies blood for patients with kidney failure.
Surgical Equipment
Surgical equipment includes tools and machines used in operating theaters for performing surgical procedures.
1. Operating Tables
Adjustable tables that allow positioning for various surgeries.
2. Anesthesia Machines
Administer and monitor anesthesia gases during surgeries.
3. Surgical Lights
Provides high-intensity, shadow-free lighting for visibility during procedures.
4. Electrosurgical Units
Used to cut or coagulate tissue using high-frequency electrical currents.
5. Sterilizers (Autoclaves)
Eliminates bacteria, viruses, and fungi from surgical instruments through steam or dry heat.
Durable Medical Equipment (DME)
These are long-term use tools that support patient mobility, safety, or recovery.
Common DME Includes:
- Hospital beds
- Wheelchairs
- Crutches and walkers
- Patient lifts
- Bedside commodes
DME is essential for patient comfort and mobility, both in hospitals and home care settings.
Emergency and Critical Care Equipment
Emergency rooms and ICUs are equipped with advanced machinery to handle life-threatening situations.
Examples Include:
- Suction machines: Clears airways
- Crash carts: Mobile unit with emergency drugs and equipment
- Ambu bags (BVMs): Manual resuscitation
- Portable monitors and defibrillators
These tools enable quick responses to sudden emergencies and help stabilize critical patients.
Pediatric and Neonatal Equipment
Hospitals have specialized tools for newborns, infants, and children.
Includes:
- Infant incubators: Maintain temperature and humidity for premature babies
- Phototherapy units: Treat neonatal jaundice
- Pediatric ventilators: For respiratory support
- Baby warmers: Provide warmth immediately after birth
These tools are adjusted for size, sensitivity, and developmental needs of young patients.
Sterilization and Sanitation Equipment
Infection control is a core pillar of hospital safety. Hospitals use a wide range of cleaning and sterilization tools.
Examples:
- Autoclaves: For instrument sterilization
- UV sterilizers: Disinfect rooms or tools
- Disinfection robots: Automated sanitizing of hospital rooms
- Sanitizer dispensers and air purifiers
Hospitals also employ strict protocols to keep surfaces, tools, and spaces infection-free.
Communication and IT Equipment
Modern hospitals are integrating digital tools to streamline operations and enhance patient care.
Includes:
- Electronic Health Record (EHR) systems
- Nurse call systems
- PACS (Picture Archiving and Communication Systems)
- Telemedicine platforms
These technologies improve coordination, reduce errors, and make healthcare more accessible.
Equipment Maintenance and Calibration
Hospital equipment must undergo regular servicing to ensure safety and accuracy.
Standard Maintenance Includes:
- Daily functional checks
- Scheduled calibration
- Software updates
- Emergency backup systems
- Biomedical engineering team support
Hospitals often have dedicated departments for biomedical equipment maintenance.
Equipment Safety Standards and Regulations
All hospital equipment must adhere to national and international safety standards.
Regulatory Bodies:
- FDA (U.S. Food and Drug Administration)
- ISO (International Organization for Standardization)
- CDSCO (Central Drugs Standard Control Organization – India)
- NABH (National Accreditation Board for Hospitals – India)
Regular audits and certifications ensure compliance with safety protocols.
Challenges in Hospital Equipment Management
Common Issues:
- Equipment downtime
- Lack of trained operators
- Delayed repairs
- Budget constraints
Solutions include:
- Equipment tracking systems
- In-house biomedical teams
- Vendor contracts for maintenance
- Staff training and usage protocols
Conclusion
Hospital equipment is the backbone of modern healthcare. From diagnostics to life support and mobility assistance, each piece of equipment plays a pivotal role in saving lives, enhancing recovery, and maintaining hospital efficiency.
As technology evolves, so does hospital equipment—becoming smarter, safer, and more accessible. For patients, understanding this equipment can offer reassurance and a sense of control during their hospital stay.
In short, the right equipment, used correctly, at the right time, can make all the difference in a patient’s healthcare journey.
FAQs
1. Why is it important to understand hospital equipment as a patient or caregiver?
Understanding hospital equipment helps reduce anxiety, improves communication with healthcare providers, and empowers you to participate in care decisions.
2. Who is responsible for maintaining hospital equipment?
Most hospitals have a biomedical engineering department responsible for the repair, calibration, and upkeep of medical equipment.
3. How do hospitals ensure that equipment is safe to use?
Hospitals follow strict maintenance schedules, calibration routines, and safety checks as per regulatory standards. Many undergo third-party audits for accreditation.
4. Are patients allowed to bring their own medical equipment to the hospital?
It depends on the hospital’s policy. Some may allow personal CPAP machines or wheelchairs, but they must be inspected and approved by hospital staff.
5. What happens if critical hospital equipment fails during treatment?
Hospitals have backup systems (e.g., manual ventilators, generator power) and emergency protocols to handle equipment failure without compromising patient safety.